HIV-AIDS and Cervical Cancer: Understanding the Link, Symptoms, and Treatments

HIV and cervical cancer, Cervical cancer symptoms, HIV/AIDS and cancer risk, Cervical cancer treatment, HPV and cervical cancer, AIDS-defining malignancies, Pap smear and cervical cancer, Cervical cancer in HIV-positive women, Immune system and cervical cancer, HPV vaccination and cervical cancer prevention, Antiretroviral therapy for HIV, Cervical cancer diagnosis and treatment, HPV infection and cervical cancer risk, Treatment for cervical cancer in HIV-positive patients, Cervical intraepithelial neoplasia (CIN), Screening for cervical cancer, HIV impact on cancer progression, AIDS-related cancers, Prevention of cervical cancer in HIV patients, Managing cervical cancer with HIV
Introduction: HIV/AIDS and cervical cancer are two significant health conditions that, when combined, present unique challenges to both diagnosis and treatment. In recent years, cervical cancer has been classified as one of the AIDS-defining malignancies, marking an important intersection between HIV and cancer. It’s crucial to understand how HIV/AIDS affects the progression of cervical cancer, the symptoms of this cancer, and the available treatment options to ensure timely interventions and improve the quality of life for those affected.
Understanding the Cervix and Cervical Cancer
The cervix is the lower, tubular portion of the uterus in females, located at the top of the vagina. It connects the uterus to the vaginal canal. Under normal conditions, the cervix is lined with cells that are constantly renewing themselves. However, in some cases, these cells can become abnormal and eventually develop into cancer.
Cervical cancer begins in the cells of the cervix, often in the transformation zone, where the squamous and columnar cells meet. This area is particularly susceptible to infection by the human papillomavirus (HPV), which is a known precursor for the development of cervical cancer.
When discussing HIV/AIDS and its connection to cervical cancer, it is important to note that HIV-positive women are at significantly higher risk of developing cervical cancer compared to those without HIV. HIV weakens the immune system, impairing the body’s ability to fight infections such as HPV, which can lead to abnormal cell changes in the cervix, increasing the risk of cervical cancer.
The Link Between HIV/AIDS and Cervical Cancer
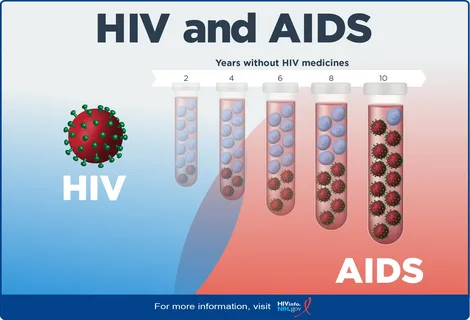
Individuals living with HIV are more likely to develop cervical cancer due to their compromised immune systems. HIV weakens the immune system by attacking and destroying CD4 cells, which are essential in the body’s immune response. As the immune system becomes increasingly compromised, it becomes more difficult for the body to fight off infections such as HPV, a primary risk factor for cervical cancer.

In people with HIV/AIDS, the ability to clear an HPV infection is significantly reduced, which increases the risk of persistent infection. Persistent HPV infections can lead to abnormal changes in the cervical cells, known as dysplasia. Over time, if these changes are left untreated, they can progress into cervical cancer.
Furthermore, women with HIV/AIDS are more likely to develop cervical intraepithelial neoplasia (CIN), a pre-cancerous condition that, if left unchecked, can progress to invasive cervical cancer.
The association between HIV and cervical cancer highlights the importance of regular screening and early intervention for women living with HIV. This intersection of diseases emphasizes the need for integrated care that addresses both HIV treatment and cancer prevention.
Symptoms of Cervical Cancer
Cervical cancer, especially in its early stages, may not present any noticeable symptoms. This is why regular screening is critical for detecting the disease early. However, as the cancer progresses, several symptoms may begin to manifest. It is important to note that the presence of one or more of these symptoms does not necessarily indicate cervical cancer but may point to other gynecological conditions as well.
Early symptoms of cervical cancer may include:
- Abnormal Vaginal Bleeding: This is one of the most common symptoms of advanced cervical cancer. Women may experience bleeding between periods, after sexual intercourse, or after menopause.
- Unusual Vaginal Discharge: This discharge may be watery, thick, and may have a foul smell. In some cases, it may contain blood.
- Pelvic Pain: Pain during intercourse or pain in the pelvic region may occur, which could be a sign that the cancer has spread beyond the cervix.
- Painful Urination or Blood in Urine: If the cancer spreads to the bladder, it may cause pain during urination or blood in the urine.
- Swelling in the Legs or Lower Back Pain: If the cancer spreads to the lymph nodes or other organs, it may cause swelling in the legs or persistent lower back pain.
It is important to understand that these symptoms may also be caused by other, less severe conditions such as infections or fibroids. However, if you experience any of these symptoms, it is essential to seek medical advice promptly.

How HIV Affects the Symptoms of Cervical Cancer
HIV-positive women may experience the symptoms of cervical cancer more intensely, and the disease may progress more rapidly due to a weakened immune system. Moreover, immunosuppression caused by HIV can make it more difficult for the body to repair abnormal cervical cells or fight the development of cervical cancer.
In addition to the usual symptoms, HIV-positive women may also face additional challenges related to the side effects of HIV medications. Antiretroviral therapy (ART), used to manage HIV, can have its own set of side effects, which may further complicate the diagnosis and treatment of cervical cancer.
Diagnosis of Cervical Cancer
Early detection of cervical cancer can significantly improve the chances of successful treatment. The most effective method for early detection is through cervical screening. Women who are sexually active or over the age of 25 should regularly undergo screening tests, regardless of their HIV status.
- Pap Smear (Pap Test): The Pap smear is the most common screening test for cervical cancer. During this test, a healthcare provider takes a small sample of cells from the cervix. These cells are then examined under a microscope to check for any abnormalities, such as dysplasia or HPV infection. If abnormal cells are detected, further testing and follow-up procedures will be required.
- HPV Testing: Since HPV infection is the primary cause of cervical cancer, testing for the presence of high-risk HPV strains is another important screening method. HPV testing can be done alongside a Pap smear or as a separate test.
- Colposcopy: If abnormal cells are found during a Pap smear, a colposcopy may be performed. This procedure involves using a special microscope (colposcope) to closely examine the cervix and take biopsies of any suspicious areas for further analysis.
- Biopsy: A biopsy involves removing a small piece of tissue from the cervix for laboratory analysis. This test is used to confirm the diagnosis of cancer or precancerous changes.
- Imaging Tests: In cases where cervical cancer is suspected to have spread, imaging tests such as CT scans, MRI, or PET scans may be used to assess the extent of the cancer and check for metastasis to other organs.
Treatment of Cervical Cancer in HIV-Positive Patients
The treatment of cervical cancer depends on various factors, including the stage of the cancer, the patient’s overall health, and the presence of HIV. In general, treatment for cervical cancer may involve surgery, radiation therapy, chemotherapy, or a combination of these.
- Surgical Treatment: The most common treatment for early-stage cervical cancer is surgery. Conization, a procedure where a cone-shaped piece of tissue is removed from the cervix, may be performed to treat precancerous lesions or early-stage cancer. In more advanced cases, a hysterectomy (removal of the uterus) may be necessary.
- Radiation Therapy: If the cancer has spread to other parts of the body or surgery is not an option, radiation therapy may be used to destroy cancer cells. Radiation can be used alone or in combination with chemotherapy.
- Chemotherapy: Chemotherapy uses powerful drugs to kill cancer cells or stop their growth. If the cancer has spread to other organs, chemotherapy may be the primary treatment. Common chemotherapy drugs used to treat cervical cancer include cisplatin and paclitaxel.
- Antiretroviral Therapy (ART): Women living with HIV are typically treated with antiretroviral drugs (ART), which help manage the virus and prevent further immune system damage. ART is essential in helping the immune system function better, which in turn supports the body’s ability to respond to cancer treatment. ART can also help reduce the risk of HIV-related complications during cancer treatment.
- Supportive Care: Supportive care, including pain management, nutrition support, and psychological care, is also a critical component of treatment. For HIV-positive individuals, managing the side effects of both cancer treatments and antiretroviral drugs is essential.

Prevention and Screening
Prevention is key to reducing the risk of both HPV infection and cervical cancer. The most effective preventive measures include:
- HPV Vaccination: The HPV vaccine is safe and effective in preventing infection from the strains of HPV most commonly associated with cervical cancer. Vaccination is recommended for both girls and boys, ideally before they become sexually active.
- Regular Cervical Screening: Women should have regular Pap smears and HPV tests to detect cervical abnormalities early. Early detection of dysplasia or HPV infection can prevent the progression to cervical cancer.
- Use of Condoms: Using condoms during sexual intercourse can reduce the risk of HPV and other sexually transmitted infections (STIs), which can contribute to the development of cervical cancer.
- Maintaining a Healthy Immune System: For women living with HIV, maintaining a high CD4 count through ART is crucial in preventing HPV infections and reducing the risk of cervical cancer. Regular HIV care and treatment are essential.
Conclusion
The connection between HIV/AIDS and cervical cancer highlights the importance of early detection, regular screening, and prompt treatment. Women living with HIV are at a higher risk of developing cervical cancer due to their compromised immune systems.